What do Casey Kasem, Christopher Reeve and Muhammad Ali have in common? They all died of sepsis: a rapid, potentially deadly reaction that affects about 1 million Americans each year.
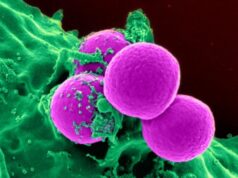
In the medical community, sepsis can be a scary word. It means the body’s own immune system is going into overdrive trying to kill a blood-borne bacterial infection. It’s an easily treated condition, but if left untreated can kill a person in two days.
The even scarier part? Normal methods of detecting sepsis take at least that long.
But researchers in the Texas Tech University Department of Chemistry & Biochemistry have found a new way to significantly reduce that detection time, giving medical professionals a greater window of time in which to treat the patient.
“Normally when you detect sepsis, you do it through bacterial culture; that takes two days on the short end to 15 days on the long end,” said Dimitri Pappas, an associate professor of chemistry. “Most people die of sepsis at two days. The detection currently is on the exact same time scale as mortality, so we’re trying to speed that up.
“Instead of the bacteria, we’re looking at the body’s immune response to those bacteria, because that’s what you really care about. The bacteria cause the infection, but it’s the body’s response that causes sepsis.”
Find your dream job in the space industry. Check our Space Job Board »
Working in a field known as microfluidics, Pappas and graduate student Ye Zhang recently filed a provisional patent for a tiny glass-and-plastic chip that can confirm a sepsis diagnosis in just four hours.
“With early diagnosis, appropriate treatments can be conducted in time and sepsis progression can be controlled,” Zhang said. “Many lives can be saved with this project by shortening diagnosis time and speeding up intervention time.”
In a nutshell, sepsis is a runaway immune response, wherein the body’s act of saving itself can actually be lethal. It begins with what’s called systemic inflammatory response syndrome — that’s the body ramping up the immune system to fight the bacteria. From there, it progresses into sepsis and eventually septic shock, in which blood pressure plummets, organs fail and eventually the patient dies.
“It is estimated there are 1 million new cases of sepsis in hospitalized patients per year in the United States,” said Dr. John Griswold, professor and chair emeritus in the Department of Surgery at the Texas Tech University Health Sciences Center. “Sepsis is the leading cause of death in intensive care units in the United States, and patients with the diagnosis of sepsis have a minimum of a 30 percent chance of dying of their disease; if their vital organ systems — brain, heart, lungs, liver, kidneys — are affected, they have a 70 percent chance of dying. The elderly have the highest rate and, in some studies, death is over 85 percent in those over the age of 75.”
In addition to mortality, sepsis can result in amputation of limbs or prolonged hospitalization. Griswold said it’s considered one of the most costly diseases in health care, amounting to a staggering $22 billion to $25 billion each year, a cost that’s increasing by 11 to 12 percent each year.
“The way they treat sepsis right now is through a massive antibiotic administration,” Pappas said. “That’s good, actually, but if you do it prophylactically and when it’s not needed, you’re basically helping create drug-resistant bacteria. So there’s a need to detect sepsis and to treat it but not to over treat it as well, because over treating it leads to additional problems.”
The chips are designed to look for the activation of certain white blood cells, which would indicate the immune system was going to work to fight the infection. The chip requires less than a drop of blood for an accurate test, so doctors can test multiple times to determine the occurrence of sepsis as well as retest periodically after administering antibiotics to make sure the body’s response is returning to normal.
At this point, all testing has been done with the help of stem cells. Because of the chip’s success, the next step is to test with human blood. And thanks to a collaboration with Griswold and the Health Sciences Center, Pappas will start enrolling patients in November.
“Through the ingenuity and creativity of our faculty, a solution to this problem is now within grasp,” said Guy Loneragan, interim vice president for research. “This ingenious discovery illustrates the value to society of the continued commitment of Texas Tech to encourage and celebrate intellectual curiosity in research and scholarship. This discovery can transform medical care and, in time, could save countless lives.”
Source: Texas Tech University