In news with several layers of weird, researchers have determined that the mix of bacteria that live inside your nose — yes, there are organisms living inside your nose — correlates with the type and severity of cold symptoms you develop.
For example, people whose noses are rich in Staphylococcus bacteria had more severe nasal symptoms than cold sufferers who have less staph, new research shows. That’s despite their colds being caused by the exact same strain of virus.
The researchers found that the bacteria in volunteers’ noses fell into six different patterns of nasal microbiomes. The different patterns were associated with differences in symptom severity. The compositions also were found to correlate with viral load — the amount of cold virus inside the body.
The discovery surprised even the longtime cold researchers who made it. “The first surprise was that you can kind of identify these different buckets that people kind of fit into, and then the fact that the buckets seem to have some impact on how you respond to the virus and how sick you get was also interesting,” said Ronald B. Turner, MD, of the University of Virginia School of Medicine. “There were effects on virus load and how much virus you shed in your nasal secretions. So the background microbiome, the background bacterial pattern in your nose, had influences on the way that you reacted to the virus and how sick you got.”
The Role of Your Nose Inhabitants
Find your dream job in the space industry. Check our Space Job Board »
To be clear, the microorganisms living in your nose aren’t causing the cold. The cold itself is caused by a cold virus, of course. And the researchers can’t say whether the microorganisms in your nose are actually responsible for the differences in symptom severity. Maybe, but more research would need to be done to determine that.
“What we’re reporting is an association, so it’s entirely possible that the fact that you have staph in your nose and you have more symptoms is not directly related,” Turner said. “It may well be that there’s some underlying host characteristic that makes you likely to have staph in your nose and also makes you more likely to become ill.”
For example, your genes might be responsible both for the composition of your nasal microbiome and for your reaction to the cold virus. Or it may be much more complicated than that. “Whether there are environmental characteristics that also influence it — whether you’re exposed to pollution or whether you’re allergic or whether any number of things might impact it — I don’t know,” Turner said. “But I suspect there is some interaction among the host and the environment and the pathogen that determines what you end up with.”
The researchers tested152 study participants’ nasal microbiomes before and after giving them the cold virus, ruling out the possibility that the virus or the resulting sickness was altering the composition of the microbiome significantly.
Could Probiotics Shorten Your Cold?
Turner and his colleagues were interested to see whether giving people probiotics — beneficial bacteria — might improve their cold symptoms or affect the composition of their nasal microbiomes. The answer? Nope.
The researchers gave study participants a probiotic to drink. Not only did it not affect the microbiomes in their noses, it didn’t have much effect on the microbiomes in their stomachs, either. “We can detect the probiotic in the gut very frequently. Not in everybody, but very frequently,” Turner said. “It didn’t really dramatically influence the microbiomic pattern of the gut. So it’s not like the probiotic alters the microbiome of the gut in any substantial way.”
It’s possible that administering a probiotic directly to the nose, such as through a spray, could have more effect. But Turner, who has been researching colds for decades, is skeptical that it would make a big difference.
“It’s not going to be so simple, I don’t think, as saying, ‘OK, what happens if you give a probiotic?'” he said. “One of the things that would be interesting to ask, and this would be a completely different study, is, what happens if you give antibiotics? Can you change the nasal flora by giving antibiotic? And is that a good thing or is that a bad thing? Those are all unknowns.”
Findings Published
The researchers have published their findings in Scientific Reports. The work represented a collaboration of UVA, DuPont Nutrition & Health and 4Pharma Ltd. The research team consisted of Markus J. Lehtinen, Ashley A. Hibberd, Sofia Männikkö, Nicolas Yeung, Tommi Kauko, Sofia Forssten, Liisa Lehtoranta, Sampo J. Lahtinen, Buffy Stahl, Anna Lyra and Turner.
Turner and other members of the research team received funding from DuPont, the maker of a probiotic used in the study.
Provided by:
University of Virginia Health System
More information:
Markus J. Lehtinen, Ashley A. Hibberd, Sofia Männikkö, Nicolas Yeung, Tommi Kauko, Sofia Forssten, Liisa Lehtoranta, Sampo J. Lahtinen, Buffy Stahl, Anna Lyra, Ronald B. Turner. Nasal microbiota clusters associate with inflammatory response, viral load, and symptom severity in experimental rhinovirus challenge. Scientific Reports (2018). DOI: 10.1038/s41598-018-29793-w
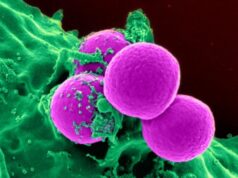
Image:
Nasal microbiomes patterns were associated with differences in symptom severity.
Credit: © Monkey Business / Fotolia