Could a slippery glob of algae hold the key to the next anti-cancer drug? According to new research into a compound produced by a unique community of blue-green algae, the answer could be yes.
The compound in question is called coibamide A, discovered eight years ago by scuba-diving scientist Kerry McPhail, Ph.D., of Oregon State University. A new study shows coibamide A has potent anti-cancer activity in mice and cell cultures that model brain tumors and triple negative breast cancer, two of the most aggressive and difficult-to-treat types of cancer.
“The chemical diversity found in nature has always been a significant source of inspiration for drug design and development, but although the medicinal properties of plants have been recognized for thousands of years, marine environments remain relatively unexplored,” said Jane Ishmael, Ph.D., associate professor of pharmacology at Oregon State University and the lead author of the new study. “We think that with this compound, nature has already found a way to target some of the specific proteins that are relevant to the growth of tumors.”
Ishmael will present this research at the American Society for Pharmacology and Experimental Therapeutics Annual Meeting during Experimental Biology2016.
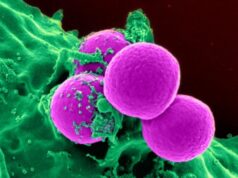
McPhail, who specializes in blue-green algae and dives all over the world in search of interesting species, collected the algae during a dive in Panama’s Coiba National Park. It turned out to be a mash-up of at least three algal species that grow together on rocks in areas with fast-moving water. In addition to Panama, similar algal communities has been found in the Red Sea and off the coast of South Africa. Blue-green algae, or cyanobacteria, have existed for at least two billion years and are one of the oldest life forms on Earth.
Find your dream job in the space industry. Check our Space Job Board »
After McPhail isolated coibamide A from the original algal specimen, it was run through a National Cancer Institute screening system that looks for potential anti-cancer activity across 60 different types of cancer. Coibamide A showed a pattern of activity unmatched by any other compound, suggesting it might be able to fight cancer through a mechanism of action unlike that of any existing drug.
The screening revealed coibamide A to be capable of killing many types of cancer cells, but Ishmael decided to focus subsequent studies on two types in particular — brain tumors, or glioblastomas, and a breast cancer subtype known as triple negative breast cancer.
“Patients with many other types of cancer already have some really excellent treatment options, so we were interested in focusing on some of the kinds of cancer that haven’t had as much success with pharmacological development,” said Ishmael. “For many brain tumors, for example, there are very few options and the prognosis has remained grim for many years.”
The team’s experiments in cell cultures, conducted with funding from an American Brain Tumor Association Discovery Grant, showed that coibamide A cuts off the cancer cells’ ability to communicate with blood vessels and other cells, eventually starving the cell and triggering its death. In an animal model for glioblastoma in which human tumor cells are grown in a mouse’s flank, treatment with coibamide A significantly reduced tumor size. The team’s next steps are to test coibamide A in a mouse model for triple negative breast cancer and in a mouse model for brain cancer in which the glioblastoma cells are grown in the brain instead of the flank.
Glioblastomas are particularly difficult to treat because these tumors grow exceptionally quickly and do not respond well to most available chemotherapy drugs. Surgery, followed by radiation treatment, is usually recommended, but it is difficult to remove every last cancer cell and the tumor often rebounds. One challenge in developing drugs to fight brain tumors is that agents must be able to cross the blood-brain barrier, a filtering mechanism that only allows certain types of substances to enter the brain. It is not yet clear whether coibamide A would be able to cross the blood-brain barrier, an aspect the team plans to investigate in the future.
Ishmael said even if coibamide A itself cannot enter the brain or turns out to have adverse side effects, knowing its structure and mechanism of action can help researchers develop new drugs that mimic coibamide A’s effects. “So far, there isn’t a drug in clinical use or in any clinical trials that works in this way. We’re using it to try to reveal a new pathway to trigger cell death in these cancer cells that have traditionally been considered very resistant to cell death,” said Ishmael.
Those research efforts recently got a lot easier when collaborators at Japan’s Kyoto University developed a method to produce coibamide A synthetically. Previously, Ishmael’s team had relied on samples isolated from natural specimens, which could not be grown in the lab and had to be harvested from marine environments. With the new synthetic form of coibamide A now available, the team hopes to move forward quickly toward developing the compound into a nature-inspired cancer drug.
Ishmael will present the findings during the Experimental Biology 2016 meeting on Wednesday, April 6.
This article originally appeared at Federation of American Societies for Experimental Biology (FASEB).